
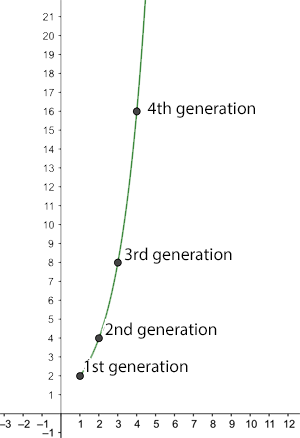
The number of new infections after n generations for R0=2.
Two things many of us will have heard about over the last few weeks are the concept of herd immunity and a number called $R_0$ (which people say as "R nought").
The basic reproduction number
Given an infectious disease, such as COVID-19, $R_0$ is the basic reproduction number of the disease: the average number of people an infected person goes on to infect, given that everyone in the population is susceptible to the disease. For COVID-19 this is currently estimated to lie between 2 and 2.5. For seasonal strains of flu, it lies between 0.9 and 2.1. And for measles it is a whopping 12 to 18.
You can see how a large enough $R_0$ leads to a rapid spread of the disease. For example, if $R_0$ is equal to 2 then a single infected person generates the following growth of new infections:
1st generation: $2$ new infections 2nd generation: $4$ new infections 3rd generation: $8$ new infections 4th generation: $16$ new infections.
Generally, there are $2^n$ new infections in the $n$th round of new infections. Assuming a person is only infectious for a week, at this rate the entire world population (7.8 billion) would be infected after slightly over 32 weeks.When the basic reproduction number $R_0$ is less than 1 a very different picture emerges. As an illustration, imagine we have $R_0=0.5.$ Now obviously, an infected person can't go on to infect half a person, but remember that this is an average: it means that 10 people can be assumed to go on to infect 5 others, or that 100 people can be assumed to go on to infect 50 others. As before let's assume there is 1 infected person to start with, then the number of new infections behaves like this:
1st generation: $0.5$ new infections 2nd generation: $0.25$ new infections 3rd generation: $0.125$ new infections 4th generation: $0.0625$ new infections.
Generally, there are $(0.5)^n$ new infections in the $n$th round of infections. This number becomes smaller and smaller as the number $n$ of generations becomes larger. A dead end for the disease.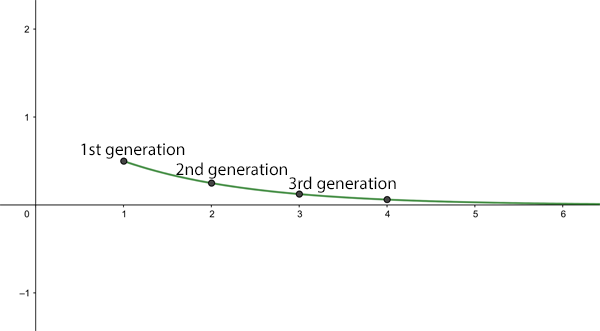
The average number of new infections after n generations for R0=0.5.
What if $R_0=1$? In this case the disease will be endemic: always present in the population, but not an epidemic.
See here for all our coverage of the COVID-19 pandemic.
The effective reproduction number
So, given that the $R_0$ of measles, or some strains of seasonal flu, is greater than 1, how come the whole world hasn't been infected with these diseases a long time ago? The reason is that $R_0$ is the average number of people an infected person goes on to infect, given that everyone in the population is susceptible. In real life, this might be the case if someone who has become infected with a disease elsewhere enters a part of the world where the disease has never been seen before, so people don't have immunity and there isn't a vaccine to protect them. An $R_0$ of $2$ then means that, at the beginning, the number of infected people will grow wildly, as we've described above.
However, once a person has recovered from the disease they will (hopefully) gain some immunity. This means that after a while we're not dealing with a totally susceptible population anymore. Indeed, there may be other reasons why some people in the population aren't susceptible: they may be immune for other reasons, or if there's a vaccine, they may have received it, or they may be isolated from the rest of the population.
In most real life situations we should be looking at the effective reproduction number of the disease, sometimes denoted by $R$: the average number an infected person goes on to infect in a population where some people are immune (or some other interventions are in place). Of course $R_0$ and $R$ are related. Writing $s$ for the proportion of the population that is susceptible to catching the disease, we have
$$R=sR_0.$$ As an example, if only half the population is susceptible, so $s=0.5$, we have $R=0.5R_0$. In this case, if $R_0$ is less than or equal to $2$, then $R$ is less than or equal to $1$ and the disease won't turn into an epidemic. The ideal aim of any intervention, be it vaccination or social distancing, is to get the effective reproduction number down to under 1.Herd immunity
What does all this have to do with herd immunity? The general idea behind herd immunity is that in a population where many people are immune a disease can't take hold and grow into an epidemic, thereby protecting people who aren't immune. The population (perhaps unfortunately called a herd ) protects vulnerable individuals.
So how many people in a population need to be immune to have herd immunity? Imagine a disease has a basic reproduction number $R_0$, which is greater than 1 so an epidemic threatens. As we have seen, if the effective reproduction number $R$ is less than 1, then the disease will eventually fizzle out. So to achieve herd immunity we need to somehow get the effective reproduction number $R$ to under 1. Since $R=sR_0$, where $s$ is the proportion of the population that is susceptible, we need
$$sR_01-1/R_0.$$ So, to achieve herd immunity we need to make sure that at least a proportion of $1-1/R_0$ of the population is immune. For an $R_0$ of 2.5, the higher end of the estimates for COVID-19, this means that we need to get at least a proportion of $1-1/2.5=0.6$ of the population immune. This translates to at least 60\%.
The herd can protect the individual.
How do we do this? Well, ideally we would do it by vaccinating at least 60% of the population. In the absence of a vaccine, we can hope that this level of immunity will be achieved naturally, by people becoming sick and then immune. But because a lot of people die of COVID-19 we can't just let the disease wash over the population, confident in the knowledge that more infections mean more immunity.
It's because we need to protect vulnerable people and our health care systems that much of the world is currently in lockdown. Ironically, lockdowns mean that many of us are not gaining immunity by having been infected, so the epidemic may spike again once social distancing measures are lifted.
So what are we to do in this worst case scenario? One option would be to remain in lockdown until there is a vaccine, but that could be over a year. Another is to go into intermitted lockdowns to keep successive spikes of the epidemic below the critical capacity of health care systems.
The truth is that at this moment nobody knows exactly what is going to happen in the future. Our most educated guesses come from mathematical models which try and predict the course of the pandemic. You can find out more about these models here. An urgent call has gone out to the scientific modelling community to help find the best exit strategies from our current predicament.
In general, our calculations above also send an important message about vaccination: it does not only protect the individual who is being vaccinated against the disease, but also those people who for some reason or other won't be vaccinated and are therefore vulnerable. Vaccination isn't just for you, it's for the whole "herd"!
This article is based on a chapter from the book Understanding numbers by the Plus Editors Rachel Thomas and Marianne Freiberger.