
Measles cases on the rise: Why this is worrying and what we can do
Brief summary
Measles cases are on the rise in the UK and epidemiologists worry that a nation-wide epidemic might occur. There is a safe and effective vaccine, but uptake among the population needs to be at least 95% if vaccination is to halt or slow down the spread because measles is extraordinarily infectious. This article explains the details.
Measles is an uncomfortable disease usually presenting as cold-like symptoms and a rash. It normally clears within 7 to 10 days, but can lead to severe complications, such as blindness, infections of the lungs and brain, and even death. Measles is known as a childhood disease because once you've had it, and traditionally most people would catch it as children, you have life-long immunity and won't catch it again. Childhood diseases are usually highly transmissible.
Why are epidemiologists worried?

A measles rash
Since October 1, 2023 there have been 1109 laboratory confirmed cases in England. England has a population of over 56 million, so 1109 cases does not seem a lot. The problem is that measles is extraordinarily infectious. Rough estimates suggest that if the disease enters a setting where everyone can catch it, a single infected person will go on to infect around 17 other people, on average.
This can lead to steep exponential growth in a population where everyone is susceptible. If we imagine that 1 person infects 17 new people, who each infect 17 new people, and so on, then as long as nothing prevents the spread, just 8 generations of infection generate over 435 million cases, far exceeding the population of the entire UK.
The average number of people an infected person goes on to infect, in a population where everyone is susceptible to becoming infected, is called the basic reproduction ratio of the disease. It's usually denoted by R0. The R0 of other familiar infectious diseases is a lot lower than 17. For seasonal flu it's roughly between 1 and 2 and for the original COVID-19 variant it was just under 3 (though for subsequent variants it was higher).
The value 17 is only a rough estimate because techniques for inferring R0 from data are not exact. Another issue is that there is no such thing as a definite value of R0 for any given infectious disease. "[Its value] depends on biological properties of the virus, for example how transmissible it is, but also on the [cultural and societal] setting," says Sebastian Funk, Professor of Infectious Disease Dynamics at the London School of Hygiene and Tropical Medicine. In a setting where people have a lot of contact with others, or are vulnerable, perhaps because of general poor health, the value of R0 is likely to be higher than in settings where people are more isolated and/or in better health.
The estimate of 17 is based on data collected in England and Wales in the 1950s and 1960s, largely before mass vaccination was introduced in the early 1960s. "Since then patterns of [social] mixing have changed," says Matt Keeling, Professor of Epidemiology at the University of Warwick. "Family sizes are smaller, class sizes are smaller, there is generally less overcrowding. [This means the value of R0 for measles in England and Wales] is now probably lower than 17 — but how much lower we don't know."
There is also concern about measles outbreaks in adults. Because people historically caught measles when they entered school, estimates of R0 are based on outbreaks among children. “Whether [the value of R0] is [17] in outbreaks amongst adults, which we haven't seen historically, [is something we] don't know," says Funk.
At the same time, outbreaks among adults are now more likely. Because today there is an effective vaccine (see below) the level of measles in the population is lower than it was in the past. As a result fewer people encountered the measles virus as children, leaving them vulnerable to catching it as adults if they are not vaccinated. This is worrying because measles infection in adults is more likely to be associated with severe symptoms than infection in children.
There is also another ominous aspect to measles, affecting both children and adults, which has only recently come to light. "Scientists have discovered that measles infection often leads to immunological amnesia where natural immunity to other infections is suppressed by measles," says Keeling. "This leaves individuals susceptible to a range of other [diseases]."
What can be done?
The good news is that there's a safe and highly effective vaccine for measles, usually given as part of the MMR vaccine for measles, mumps and rubella. People only need to be vaccinated once during their lifetime, but two doses are needed for the vaccine to be fully effective.
To protect children from as early on as possible, the NHS vaccination schedule suggests the doses be given at the ages of 1 year and 3 years, 4 months. But older children and adults aren't excluded — if they weren't vaccinated when they were younger they can receive the vaccine at any time.

The MMR vaccine is safe and effective.
The MMR vaccine works extremely well. One dose stops around 95% of measles infections among those who were vaccinated, and a second dose takes this up to around 99%. Despite this high efficacy, the high infectiousness of measles means that a lot of vaccination is necessary if we're going to eliminate measles or keep it under tight control. In its global measles and rubella plan for 2012 to 2020 the World Health Organisation (WHO) recommended that 95% of the population should ideally receive both doses of a measles vaccine.
The number can be explained using epidemiological theory. The basic reproduction ratio R0 measures the infectiousness of a disease when everyone in the population can catch it. But once some people have become immune, the disease spreads less easily. In fact, when sufficiently many people in the population are immune, any outbreak will die out by itself.
A calculation suggests how many people would need to be immune for this to happen: it's a proportion of 1-1/R0 of the population. The proportion 1-1/R0 is known as the herd immunity threshold, a term that stems from veterinary epidemiology. When this proportion is achieved, then the immunity within the herd protects vulnerable individuals. For a disease with R0=17 the herd immunity threshold works out to 94.1% of the population. Intuitively, if an infectious person would normally infect 17 new people, but 16 out of these 17 (or 94.1%) are protected then the infection cannot increase in the population.
This proportion is already high, but it's important to note that it only gives an immunity threshold, not a vaccination threshold. There's a distinction between the two because no vaccine is 100% effective: there will always be some people who've been fully vaccinated but aren't fully immune. To achieve herd immunity, we would therefore need to aim for a vaccination coverage that is higher than the idealised immunity threshold - for a disease with an R0 of 17 and a vaccine efficacy of 99%, we would need a vaccination coverage of at least 95%. (You can see the details of this calculation here.)
Another factor to consider is that not everyone in the population can receive the MMR vaccine. A crucial exception are babies under the age of 1, because they will have inherited antibodies from their mothers that can work against the vaccine. Pregnant women, people with weakened immune systems, and those who've previously had allergic reactions to ingredients of the vaccine are also advised not to receive it as it may put them at risk. With fewer people eligible to receive the vaccine, a higher proportion of those who are would need to be vaccinated to achieve herd immunity.
The 95% vaccination threshold given by WHO is a result of theoretical and practical considerations such as these. "[The picture] isn't completely black and white; it's not that you suddenly see massive outbreaks just because you're at 94%," says Funk. "But In order to completely stamp out [measles] you need a two-dose coverage of 95%."
In line with the WHO target, the aim in the UK is that at least 95% of children should have received both doses of the MMR vaccine by the time they are five years old.
What vaccination coverage do we have?
Vaccination coverage is measured using data from GPs and local authorities, but the exercise isn't entirely straight-forward. Information may get lost when people move and change GP, and new arrivals to the country may not know their childhood vaccination record or remember to pass it on to their GP.
What is clear, however, is that coverage for children falls short of the 95% target. According to official statistics only 85.2% of children in the UK had received two doses of the MMR vaccine by their 5th birthday in 2022-23. Uptake of the first dose was higher, at 92.9%. "With the [first] dose things are easier because [people] are in the system and receive all the notifications," says Funk. For the second dose it's probably more likely that notifications are not received, or that parents fail to act on them as life gets in the way.
A look at historical vaccine uptake among children gives an idea about levels of immunity among people who have since grown into teenagers and adults. The graph below shows the percentage of children having received the first dose of the MMR vaccine by the time they were two years old, each year since 1997-98.
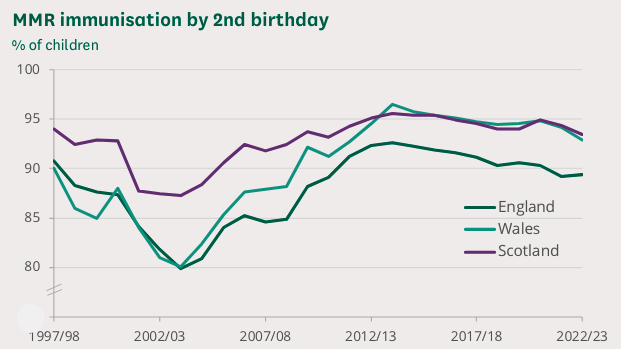
This chart shows trends in the proportion of children in England, Scotland and Wales immunised against MMR by their second birthday (ie receiving the first dose). Source: Commons Library Research Briefing on Childhood Immunisation Statistics reproduced under an Open Parliament Licence.
In some local areas the impact of the Wakefield scandal was even larger than the chart above suggests. Following an anti-vaccination campaign in the South Wales Evening Post in the 1990s, uptake in two-year olds in Swansea had plummeted to 67.5% by 2003. The dip has been linked to a measles epidemic that broke out in the area in 2012 and 2013 and affected many of those who missed their vaccinations around ten years earlier. It led to over 1,200 cases, 88 hospital visits, and the death of a 25-year old man.
Apart from the Wakefield dip, the graph shows a gradual decline in vaccine uptake over the last ten years or so. The reasons for this are hard to identify. "Vaccine hesitancy has been a problem for a while across Europe, but [it's hard to] know why," says Funk. "It could be due to scepticism around government mandates, or broader distrust of government and potentially scientists." Lingering fears about the discredited link to autism may play into the hesitancy. In addition there’s the fact that, due to vaccination, fewer of us have experienced measles ourselves, perhaps making us less concerned when it comes to vaccinating our children.
Another contributing factor, which has made some headlines, may be the pork gelatine that is used as a stabiliser in one particular type of MMR vaccine that children receive by default. Its use has been described as "disappointing" by the Vegetarian Society and may also not sit well with some faith groups. An alternative version of the vaccine, free from pork gelatine, is available and can be readily requested from GPs — see this UKSHA leaflet for more information.
Overall, the low historic vaccine uptake feeds into the worry about measles outbreaks. "The fact that vaccination uptake has been below the idealised threshold for many years means that there are now many susceptible people in the population; and the number of susceptible people is increasing year on year," says Keeling. "To make matters worse, the susceptibility is not evenly distributed over the country, but is patchy due to differences in vaccine up-take. Ideally we would require a [survey of blood samples from people] across the country to understand the distribution of susceptible people—those that have neither been vaccinated nor caught measles."
What can we expect to see?
It's impossible to predict exactly when and where the next major measles outbreak is going to occur. "Measles is very transmissible, it's very good at finding [people to infect]," says Funk. "At the same time, if you look at Swansea, it took [ten years for the dip in vaccination coverage to lead to an epidemic]. There's no particular reason for why the outbreak happened in 2012 and 2013, and not in 2005 or at some other time. There's an element of chance involved. You need the virus to be introduced into the 'right' kind of immunity for there to be an outbreak."
But even though chance has a hand in the game, mathematics gives a clear warning of what we can expect to see in the country as a whole if the level of immunity in the population continues to decrease. "Mathematical theory suggests that as the proportion of susceptible people in the population increases we will observe increasing numbers of localised outbreaks of ever larger sizes, until eventually we see a nationwide wave of infection," says Keeling. Such a nationwide outbreak occurred in France between 2008 and 2011. It saw over 22,000 reported cases of measles, nearly 5000 hospitalisations, more than 1000 cases of severe disease and ten deaths.
Such an extensive wave of infection is the real risk. "Yet the solution to the problem is simple, safe and already exists: we need to achieve high levels of vaccine uptake," says Keeling. If we can get to the recommended 95% vaccination coverage, then not only will we be able to prevent epidemics spiralling out of control— there's also a real chance of eradicating measles completely.
About this article
Sebastian Funk is Professor of Infectious Disease Dynamics at the London School of Hygiene and Tropical Medicine.
Matt Keeling is a mathematician who specialises in the spread of infectious diseases. He has worked on a number of infections from measles to influenza and from COVID-19 to plague. He has been a member of the Scientific Pandemic Influenza Group on Modelling (SPI-M) since 2008, a member of the Joint Committee on Vaccination and Immunisation (JCVI) from 2010 to 2022, and a member of the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) from 2023.
Marianne Freiberger is Editor of Plus.
This article is part of our collaboration with JUNIPER, the Joint UNIversities Pandemic and Epidemiological Research network. JUNIPER is a collaborative network of researchers from across the UK who work at the interface between mathematical modelling, infectious disease control and public health policy. You can see more content produced with JUNIPER here.
